Many individuals who come to me with ill health are caught between two places. The first is: my body is breaking down and no one seems to be able to tell me what the matter is. Symptoms are concrete, frequent, specific, and real. There is something specifically wrong with me. Why is it so hard to get a diagnosis? The second space is: I am anxious and know that stress plays a role in this illness, but it seems to me that the illness is causing the stress, not the other way around. But all my doctors tell me that it is “just” anxiety. The patient is likely to find this insulting. What is the truth?

Because of the ACEs studies on childhood trauma as a cause of adult illness we are in much better position to understand how long-term stress causes “real” illness and breakdown in our biochemical selves.
So, what are the characteristics of individuals whose nervous system is causing their illness? They are the characteristics of a nervous system that is insecure. Safe childhoods produce settled nervous systems. Unsafe ones cause a feeling of constant “where is the next blow going to come from”. These personality characteristics might be the ones you’d imagine- uncertainty, indecisiveness, reluctance to assert oneself, reluctance to go into new or unfamiliar places, social phobia or at least lots of “I-should-have-saids”. Lots of second guessing of oneself. Obsessive compulsive behaviors are attempts to find security through control. Understandably there is a wariness to trust other people. There is often a search and hunger for connection and deep desire for support and help but the nervous system is very skittish and takes offense easily so a lot of these individuals have difficulty actually getting the help they are so desperate for. The internet and availability of lots of advice via Google often lead these individuals to try and manage their illness by themselves. This is a poor choice for lots of reasons; moreover learning to trust others is a big part of the solution.
Paradoxically a person with a history of early trauma, a childhood of insecurity because of adults who didn’t listen or were domineering and unable to listen may adopt the same authoritarian personality – become a bully herself. This personality often feels more comfortable in positions of power but is constantly monitoring their competition and may have a level of paranoia and a deep instinct to undercut, disparage and demean the competition rather than collaborate. This person believes that willpower, self-discipline, competitiveness, success are the places they will find security. They are often successful in material terms but constantly insecure in that midst of that material success and drive themselves and others around them into deep levels of unhappiness.
I hope this makes sense to the reader and I hope, if you haven’t, that you read about the ACE studies. Chronically dysregulated nervous systems are costly – to the individual and to us as a society. The more we understand the way challenging events condition developing nervous systems toward chronic stress in adulthood, the better we understand how to heal the wounds of early childhood insecurity. The more we understand about healing these wounds, the more we can support the body’s capacity to heal physically.
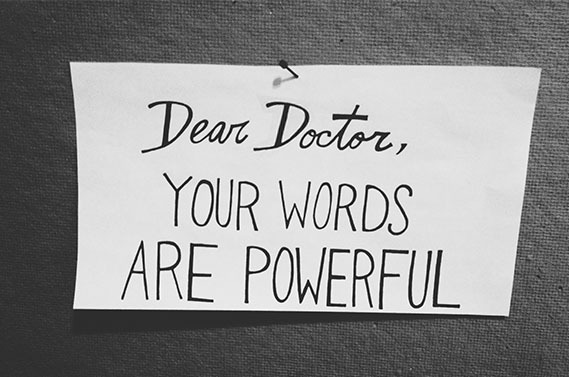
Let’s turn to the complexity of the moment when a physician says to a patient, “this is just anxiety”. I suppose one of the reasons that would be triggering is the “just”. Like it’s not real. The patient’s discouragement would be completely understandable since everything about the symptoms associated with these illnesses rooted in trauma are real. Just as real and complex is the breakdown in immunity, digestion, inflammation and detoxification, muscle tone, joint biomechanics and nerve function underlying those symptoms. In no way are these illnesses “just in the head”. Perhaps another reason a person may be insulted by such a statement would be the implication that a symptom caused by anxiety would be easy to fix, “go home and meditate” – which would reveal the physician’s naivete with regard to the responsiveness of deep-seated insecurities to simple change in habit. In truth, it’s not uncommon for physicians to feel uncomfortable in the realm of a patient’s ‘anxiety disorder’, and this discomfort can easily communicate distancing, further feeding the feedback loop of insecurity, the stress, and the physical symptoms.
Sadly, most physicians are far better equipped to treat with pills than presence. However, for symptoms to resolve, the trauma needs to be healed. Patients with trauma need most of all a steady, calm, skilled presence in their care providers.